MND Association-funded researchers from the University of Liverpool have published results in the prestigious open access journal Proceedings of the National Academy of Science. Under the leadership of Prof Samar Hasnain, the researchers identified that some TDP-43 mutant proteins hang around in the cell longer and become more stable, possibly leading to neurodegeneration in MND.
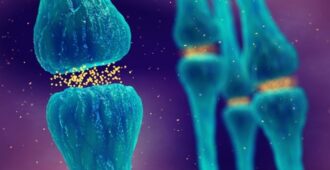
Although TDP-43 genetic mistakes are a rare cause of inherited MND (5-10% of total MND cases), scientists are especially interested in the TDP-43 protein because in the vast majority of cases of MND (irrespective of whether it was caused by an inherited genetic mistake), the TDP-43 protein forms pathological clumps inside motor neurons.

Being more stable causes MND
Normally, mutant proteins involved in neurodegenerative disease become ‘unstable’ as they are unable to perform their function. This often results in the forming of protein clumps within the motor neurones (eg this is what happens in MND caused by the SOD1 genetic mistake). However, researchers at the University of Liverpool have found that the opposite is true in TDP-43.
The mutations made the TDP-43 protein more stable, and more likely to degrade at a slower rate than normal. This ability to ‘linger’ around the cell longer than usual means that the rate of proteins made to proteins lost increases. This ultimately results in more TDP-43 protein being present in the cell, leading to neurone death and the development of MND.
Next steps
These findings further our understanding of TDP-43 and its involvement in MND. The idea that TDP-43 becomes more stable means that researchers can now begin to look at ways of disrupting this process. One way of doing this could be by developing new treatments that cause TDP-43 to break down more quickly within the cell.
Dr Brian Dickie, Director of Research Development at the MND Association said: “These surprising findings turn some of the established thinking on its head, as it suggests that TDP-43 and SOD1 forms of MND have completely contrasting mechanisms of toxicity.
“That said, they do share the same fundamental premise that mutated or altered proteins are bad for nerve cells, so finding ways of identifying ‘good’ proteins from ‘bad’ proteins and getting rid of the latter is a therapeutic strategy that needs to be pursued.”