Despite extensive research, the causes of MND remain largely unknown. Recent investigations have begun to shed light on the gut microbiome and whether it may have a role in the development and progression of MND, offering potential new avenues for understanding and possibly treating the disease.
The gut microbiome refers to the community of microorganisms, that live in the gastrointestinal tract, primarily the colon.
The gut microbiome
The ancient Greek physician, Hippocrates, often referred to as the ‘Father of Medicine’, is credited with having said, “All disease begins in the gut.” This was around 2,500 years ago but it’s only in the last 20 years or so that advancements in technology, such as DNA sequencing, have allowed us to have a much more detailed look at the link between the gut microbiome and health.
This has enabled researchers to identify many of the microorganisms living in the gut and learn much about the varied and crucial roles they play in digestion, metabolism, immunity and many other aspects of health.
However, with estimates suggesting that there are approximately 100 trillion microbial cells in the gastrointestinal tract, representing thousands of different species of bacteria, fungi, viruses and other microbes, there is still a long way to go to fully understand the gut microbiome and how it impacts the human body.
The gut-brain axis
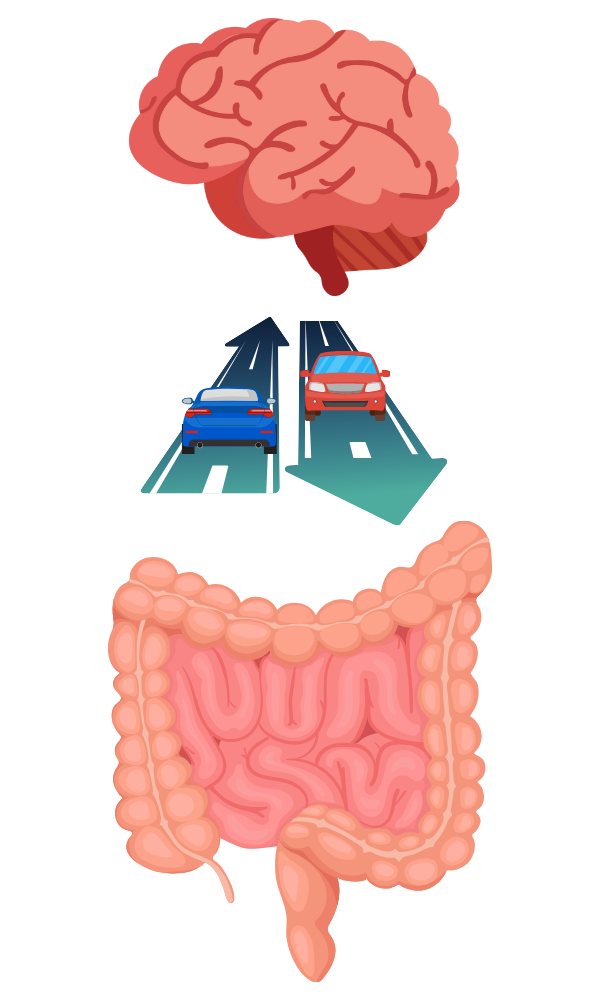
Emerging evidence suggests that the gut microbiome communicates with the central nervous system (brain and spinal cord) with information travelling back and forth, a bit like cars on a 2-way street.
This is achieved through a complex network of neural, hormonal and immunological pathways, known as the gut-brain axis.
The microbes within the gut produce substances that have an effect on our bodies.
These include vitamins, short-chain fatty acids (produced when certain bacteria ferment fibre in the diet), neurotransmitters and other products of metabolism. Via the gut-brain axis, these substances play a crucial role in regulating human biological processes, including how the nervous system works. For example, mice raised without any microbes exhibit differences in brain development and behaviour compared to those with a normal microbiome.
Research on other neurodegenerative diseases has uncovered potential links between the gut microbiome and disease. A study on people with Parkinson’s disease found that they had an imbalance in the composition of gut microbes compared to healthy controls. This included an increase in species associated with inflammation and a reduction in species with anti-inflammatory and neuroprotective properties.
Linking the gut microbiome to MND
Several studies have demonstrated alterations in the composition and function of the gut microbiome in people living with MND compared to healthy controls, as well as between people with slow versus fast disease progression. These alterations include changes in the variety of microorganisms living in the gut (microbial diversity), shifts in the numbers of specific groups of bacteria and changes associated with the chemicals that the microbes produce. For example, a number of studies have reported a reduction in bacteria that produce a type of short-chain fatty acid known as butyrate in people with MND. Interestingly, research in mice models of MND found that increasing levels of butyrate appeared to improve various gut and cell-related symptoms and increase life span, providing intriguing support for the potential link between the gut microbiome and MND.
How could the gut microbiome impact MND?

The mechanisms underlying the influence the gut microbiome may have on MND are complex, diverse and incompletely understood. However, several hypotheses have been proposed. One possibility is that changes in microbial diversity lead to widespread inflammation and immune activation, which may contribute to degeneration of the motor neurons. Another theory is that the chemicals produced by certain microbes affect the function and survival of the neurons. It has been suggested that the short-chain fatty acid, butyrate, may have neuroprotective effects and possibly help reduce inflammation.
Another theory is that butyrate may play a role in helping the gut lining stay healthy. Scientists have known for some time that the gut lining can become ‘leaky’, due to certain species of bacteria producing toxins or upsetting the balance of microbes in the gut. This allows substances, such as bacteria, toxins and undigested food particles, to pass through the lining into the blood stream.
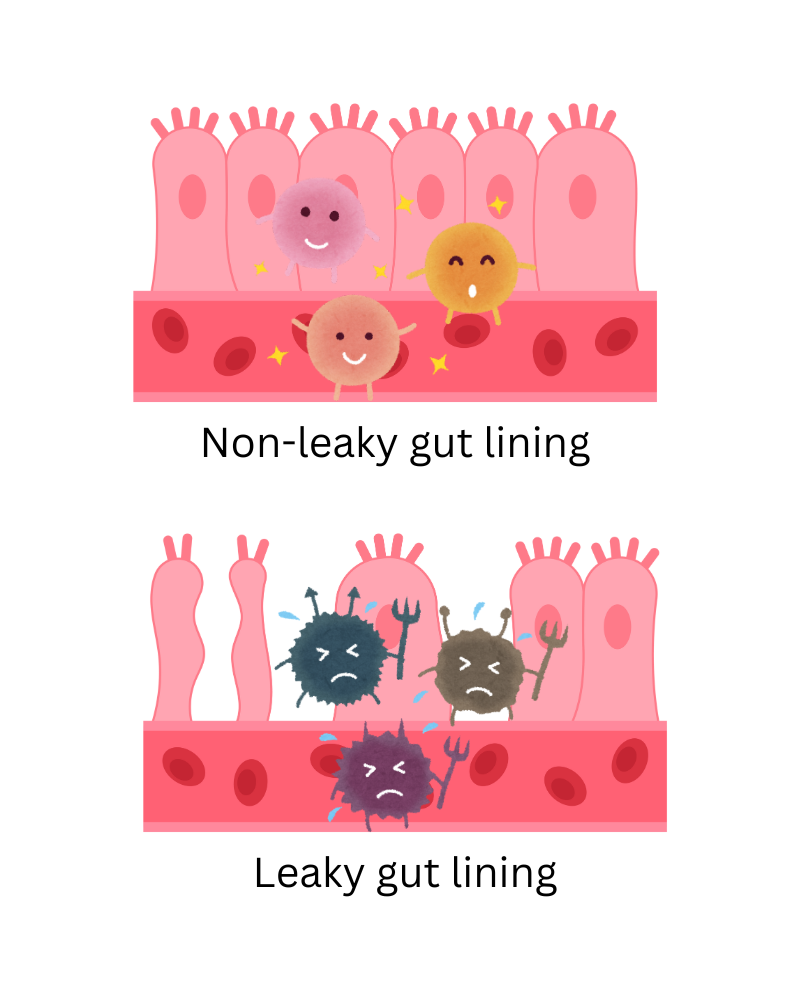
These substances can then be transported to other parts of the body where they can trigger inflammation and immune responses.
Current research on the gut microbiome in MND

A project funded by the MND Association and run by Professor Chris McDermott at the Sheffield Institute for Translational Neuroscience (SITraN), is aiming to extract DNA from stool samples from 100 people with MND to determine the microbial makeup of the samples compared to that of 100 healthy controls. The researchers will also be investigating the genes carried by the microbes in order to determine what chemicals are produced and how these may be impacting a person’s health, including the progression of their MND.
Another part of the study will collect samples from 3 people with MND and 3 healthy controls. These samples will be divided into two and grown in the lab, with one half being cultured in the presence of a probiotic, to see if this has any impact on the types and relative amounts of gut microbes. The chemicals produced by the microbes will also be analysed under the two different conditions. If key changes are found, the research team aim to run a follow-up trial to investigate the effects of taking probiotics in people with MND.

RELATED TOPIC
Research we fund | Identifying Therapeutic Targets
What this could mean
Greater understanding of the gut microbiome’s possible role in MND opens up exciting avenues for therapeutic intervention. Strategies aimed at changing the microbiome, such as probiotics, prebiotics and dietary interventions could hold promise for improving symptoms.
One randomised clinical trial in Italy is looking at whether faecal microbiota transplantation can alter the immune reaction and inflammation responses that characterise disease progression. This is a procedure in which faecal matter from a healthy donor is transferred to the gastrointestinal tract of a recipient, in this case people with early stage MND. The researchers will be looking for a change in the abundance of an immune cell known as a Treg (T regulatory cell), 3 and 6 months after the transplantation. These cells have a role in regulating the immune system and it is thought that activating them and increasing their levels may be beneficial for people with MND. The study has finished recruiting and is expected to complete in early 2025.

RELATED TOPIC
NIH National Library of Medicine | Clinical Trials
Fecal Microbiota Transplantation on Amyotrophic Lateral Sclerosis Patients (FETR-ALS)
Challenges and future directions
Whilst the emerging evidence linking the gut microbiome to MND is intriguing, many questions remain unanswered. Future research can build on these initial studies, possibly uncovering new biomarkers for early diagnosis, identifying novel targets for therapeutic intervention and ultimately improving the lives of people living with MND. As our knowledge of the gut-brain axis continues to evolve, we may yet learn that Hippocrates was right.