This is blog number 14 in our ‘Symposium Blogathon’ – counting down to the 32nd International Symposium on ALS/MND. Numbers in bold green type correspond to the code in the abstract book. Click on the number to be redirected to the full abstract (the page may take a minute to load).
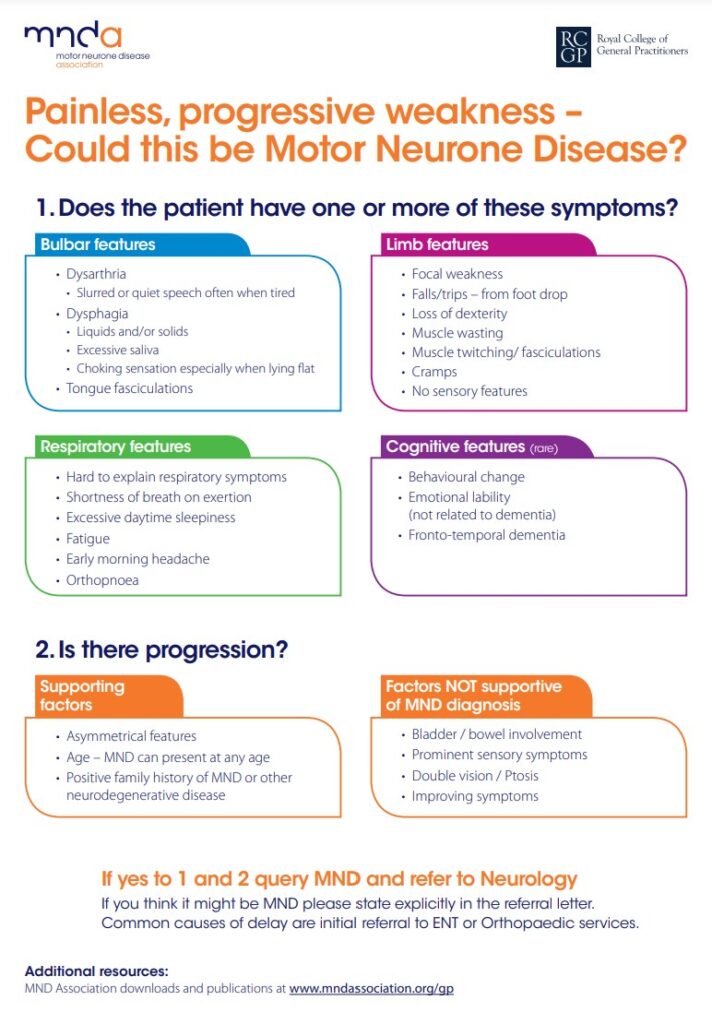
MND is difficult to diagnose early as it can mimic other neurological diseases, and early symptoms such as muscular weakness, slurred speech or a change in ability to perform everyday tasks such as buttoning clothes may be attributed to ‘getting older’.
Diagnosis of MND, however, can be further delayed as most GPs do not see many cases and may not immediately think of the disease as the cause of symptoms. If they suspect a neurological cause they will make a referral to a neurologist who will carry out appropriate tests.
At present, no one test can provide a definitive diagnosis of MND. Rather, diagnosis is made after ruling out other neurological conditions that cause similar symptoms, and a detailed physical examination. Tests may include electromyography (EMG) and magnetic resonance imaging (MRI), and laboratory tests on blood and urine to look for known biomarkers of MND.
RELATED TOPIC
Blog | 20 June 2020 | Research Dev Team
Identifying potential new diagnostic biomarkers in the blood
Because most people with MND die within two and a half years of symptom onset, it is vital that speedier and reliable diagnostic tools are developed so that treatment and symptom management can be started at the earliest possible opportunity.
MND is a rare disease, and the journey to diagnosis is often long. Patient studies have shown that those with MND are seen by 3-5 healthcare professionals and have on average 4-5 investigations prior to definitive diagnosis. Early referral to a general neurologist may not reduce the time to diagnosis. Delayed diagnosis also means that many people with MND find they are not eligible to take part in clinical trials as they fall outside the ‘x number of months since symptom onset’ eligibility criteria by the time they have their diagnosis.

In her presentation ‘The diagnostic pathway in ALS: Can we do better?’ (C24), plenary speaker Professor Orla Hardiman, from Trinity College Dublin, will talk about the challenges faced in improving diagnostic delay and how raising public awareness of MND and educating primary care practitioners may trigger early referrals to specialist clinics but may also increase the risk of ‘false positive’ presentations, limiting the availability of clinical care for people with definite diagnoses. She asks the question ‘How can we do better?’ and explores ways in which this might be achieved.
About 50% of people with MND die within 30 months of disease onset, making early diagnosis critical. An important diagnostic measure in MND is fasciculations. At present, fasciculations are detected with needle EMG, an invasive and often uncomfortable procedure. A team of researchers from Newcastle, UK, have developed a non-invasive way to detect fasciculations using MRI, called motor unit MRI (MUMRI). When comparing the results of scans in different muscle groups with healthy controls, they observed that people with MND had at least one body region with an elevated number of fasciculations compared to controls, with often at least one of the other body regions unaffected. This is in line with the variety of disease onset known in MND (IMG-15).
RELATED TOPIC
Blog | 5 November 2020 | Research Dev Team
SPiQE – new analytical tool digs deeper into fasiculations
In the USA, the average time from weakness onset to diagnosis is 11.5-15 months, during which a patient sees 3-4 medical providers prior to diagnosis confirmation. Reducing the time to initial MND neurologist consultation will greatly reduce diagnostic timelines. To this end, researchers in the USA developed the thinkALS tool to increase MND education and awareness among general neurologists in the US, with the aim of promoting early MND suspicion and improve efficiency of early referrals to MND multidisciplinary clinics for diagnosis confirmation and treatment. thinkALS was based on the Red Flag tool targeting primary care physicians, that was developed by the MND Associations in the UK and Australia (CMS-03).
Refining prognosis
Prognosis is defined as a likely course of a medical condition. ALS/MND is a progressive fatal neurogdegenerative disease, and individual prognosis can be highly variable. Several prognostic factors are known, such as site of onset (bulbar or limb), age at symptom onset, delay from onset to diagnosis, and the use of riluzole and non-invasive ventilation (NIV).
Currently, measures of clinical progression are the standard for monitoring disease progression. The most widely used measure is the ALSFRS-R. Other measures focus on more specific symptoms of the disease, including motor neurone loss, reduced breathing ability or assessment of behaviour and thinking abilities.
Because the way in which MND develops and progresses differs so widely between people living with the disease, the development and validation of ways in which to predict progression is a recognised research priority.
In his oral presentation, Mr Remko van Eenennaam, from the UMC Utrecht Brain Centre in the Netherlands, talks about ‘Discussing personalised prognosis of survival in ALS: A qualitative study of experiences of patients, caregivers and physicians’ (C13). He explores experiences of people with MND, caregivers and physicians based on the ENCALS prediction model which offers people with MND the opportunity to receive a personalised prognosis of survival at diagnosis (if they want it). Overall, patients and caregivers reported positive and reassuring effects on their mental wellbeing and indicated that it helped them to regain some control and plan for the future. Patients were keen to express that how the message was communicated was as, or more, important than the message itself (a good or bad prognosis), and that quality of life mattered more than quantity of time left.
Pauses in progression?
MND progression is known to be highly variable across patients. Given its relentless nature, the functional decline is usually expected to be continuous. However, previous studies using the revised ALS Functional Rating Scale (ALSFRS-R) showed that about 25% of people with MND experience at least one 6-month pause and that such pauses could be even longer in a smaller percentage of cases.
In their study, researchers from Italy assessed the frequency and prediction of plateaus in MND progression as assessed by the Medical Research Council (MRC) Scale, which grades muscle power on a scale of 0-5 in relation to the maximum expected for that muscle. According to MRC Scale scores, of those people with MND tested, 122, 71, and 59 experienced a plateau lasting at least 6,12, and 18 months respectively. ALSFRS-R scores revealed similar estimates. Because these findings suggest that plateaus in MND progression are not infrequent, they should be taken into account in both the clinical and experimental settings (DSP-13).
Stay informed
If you have come across this blog through the Symposium website, or a general search please subscribe (see top right hand corner of page) and you’ll be notified every time we upload a new article.
You can follow our research account on Twitter. We tweet about up to the minute research and will be tweeting throughout the Symposium – #alsmndsymp #drivingmndresearch
Take a look at the schedule of blogs for November as we continue counting down to the 32nd International Symposium on ALS/MND with our ‘Symposium Blogathon’.
To listen to talks live, take part in the Q&As and visit the live poster sessions, register for the International Symposium now.