This blog is part of our Symposium Spotlight series, where we’re looking back on some of the research that was presented at the 33rd International Symposium on ALS/MND. Today we’re taking a closer look into plenary speaker Dr Michael Benatar’s talk that he gave at the 33rd symposium’s session on disease presentation and risk. ALS is the most common form of MND and these terms are used interchangeably in this blog.
MND remains difficult to diagnose due to the initial symptoms of the disease being similar to those seen in other neurological conditions. As there is no specific test for MND, other conditions that may cause these symptoms have to be ruled out before the clinician can be sure someone has MND. This means that, on average, people receive a diagnosis of MND a year after the initial onset of symptoms which can prevent people from getting treatment and care in the very early stages of disease. It has been suggested that there might be a pre-symptomatic stage of the disease, where the disease is active and occurring within a person but no symptoms are showing. There is currently little research in this area and a lack of evidence of a pre-symptomatic stage of MND. However, if it can be shown that there is a pre-symptomatic stage which can be measured, this could be very useful in helping people with MND to get treatment as early as possible.
Dr Michael Benatar, from the University of Miami, has been looking into this by studying the development of MND and how the disease presents in people who have a high risk of developing it. In his talk ‘Mild motor impairment and prodromal markers’ (C14), he discussed how the Pre-symptomatic Familial ALS (Pre-fALS) study has helped to change the way MND is thought of and provided evidence of pre-symptomatic stages of the disease.

What is the Pre-fALS study?
The Pre-fALS study is a long-term study of people in the US who have a family history of the disease and are carrying a gene mutation that puts them at an increased risk of developing MND. The study is currently observing around 220 people to help us understand more about changes that occur in MND before symptoms appear. It aims to investigate biomarkers that may provide evidence of a pre-symptomatic stage of the disease. These biomarkers could indicate if the person will develop MND and may help to uncover whether there are ways to predict when someone might change from being pre-symptomatic to showing clinical symptoms.
What has been found so far?
Dr Benatar and the team have found that a biomarker called Neurofilament Light chain (NfL) increases in some people in the months to years before symptoms of the disease develop. As NfL increases when neuron damage is occurring, this suggests that the disease is already active in people before symptoms appear. These findings provide support for a pre-symptomatic stage of MND where neuron damage has begun but is not yet severe enough for clinical symptoms to develop.
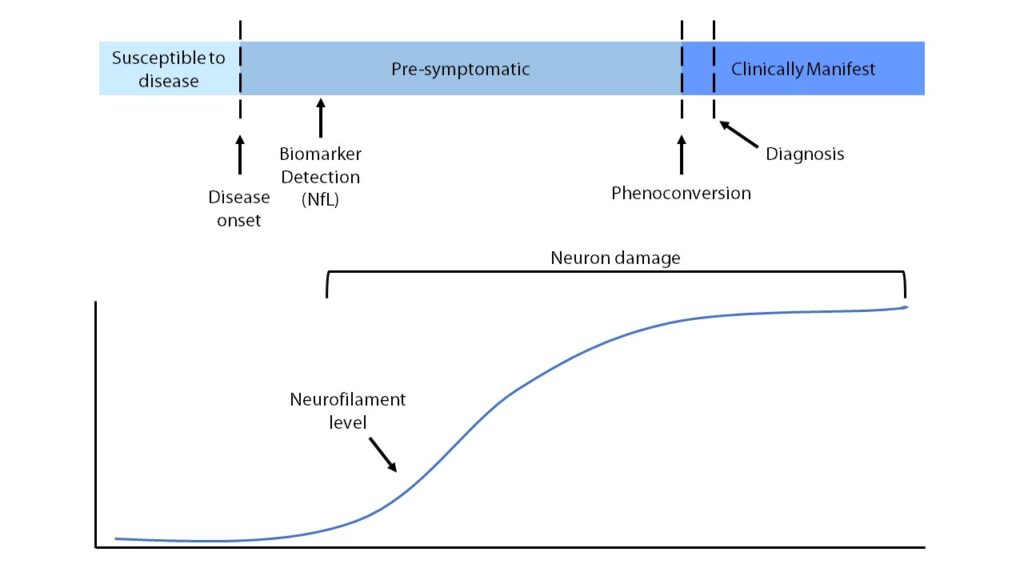
The results of the Pre-fALS study suggest that clinicians may be able to monitor people who are known to be at a higher risk of developing MND and observe when someone changes from being pre-symptomatic to having clinical symptoms (phenoconversion). Being able to study the point of phenoconversion will help researchers and clinicians to understand more about the underlying biological changes that are happening during this stage of the disease.
This study has also helped to uncover some early signs of disease activity that show in the pre-symptomatic stage and could suggest that someone will go on to develop MND. These early signs are called mild motor impairments.
RELATED TOPIC
Blog | 24 June 2022 | Charlotte Roy
Delving deeper into neurofilament light chain
What is mild motor impairment?
Mild motor impairments are thought to be movement related symptoms or changes seen in electromyography tests (measuring the health and function of nerves/muscles) that can’t be considered normal but aren’t severe enough to make a diagnosis of MND. These small motor abnormalities can sometimes be observed in people before they go on to develop full symptoms of the disease but they might not always be present before MND fully develops. Some people may not have mild motor impairments but may display other early signs of the disease. The pre-symptomatic phase can also show as mild cognitive impairment or mild behavioural impairment where changes in the way someone thinks and behaves occur before symptoms of the disease develop.
What might the stages of pre-symptomatic disease be?
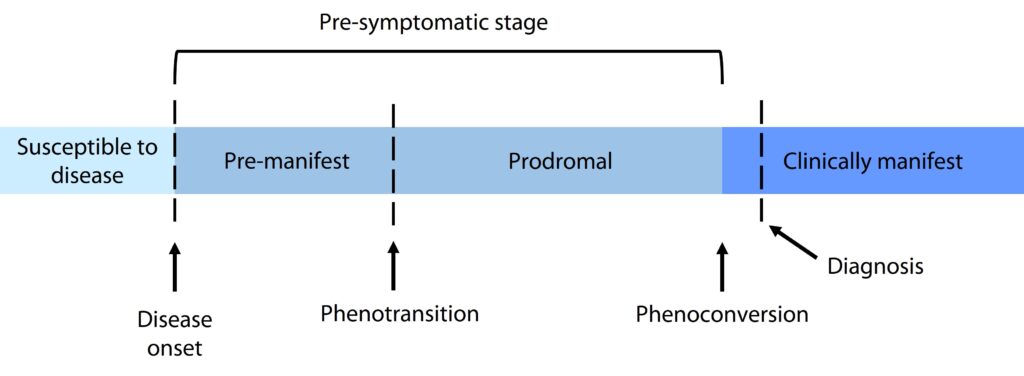
The pre-symptomatic stage of MND has been suggested to vary between people and could last anywhere from a few months to a few years before symptoms begin. It is thought that the length of this stage might be different for different gene mutations. The pre-symptomatic stage could be so short that it is missed because symptoms develop so quickly, or symptoms could develop very gradually and the pre-symptomatic stage could last for years. Dr Benatar’s research has suggested that there might be two sub-stages of disease within the pre-symptomatic stage, called pre-manifest and prodromal stages. Pre-manifest is where higher levels of NfL are found but no signs of the disease are seen and prodromal is described as higher levels of NfL with some early signs of the disease, such as mild motor impairment, mild cognitive impairment or mild behavioural impairment.
What does this mean?
The results of the Pre-fALS study have shown that the NfL biomarker can be used to detect premanifest disease in people who are at high risk of developing MND. They can then be closely monitored for mild motor, mild cognitive and mild behaviour impairments to observe when they transition into the prodromal phase. This may help with earlier diagnoses and earlier delivery of treatments for people who develop MND.
The discovery of changes in NfL occurring in the pre-symptomatic stage has led to the first pre-symptomatic clinical trial in MND. The ATLAS trial of an SOD1 gene therapy called Tofersen is recruiting 150 people with certain SOD1 gene mutations, who do not have symptoms of the disease. One of the aims of the trial is to investigate whether treatment with Tofersen in the pre-symptomatic stage can delay the onset of clinical symptoms. It will also be assessing whether pre-symptomatic treatment with this gene therapy can slow progression of the disease when symptoms do develop.
RELATED TOPIC
Blog | 21 July 2021 | Eleanor Green
Updates on Tofersen Trials for SOD1-MND
The findings from the Pre-fALS study so far provide evidence of a pre-symptomatic stages of MND where the disease is active in people before symptoms appear. These promising results also suggest that these stages of the disease are measurable using the biomarker NfL, meaning there is potential to monitor people at higher risk of developing MND for early signs of the disease, which could lead to earlier diagnoses and treatment.
The Pre-fALS study wouldn’t have been possible without the dedication, generosity and commitment of the entire MND community. Thank you to everyone who participated in this research and helped make these findings possible.