Researchers identify that loss of nerve signalling may be an early sign of MND
Published in Nature Communications on 12 January 2015, Association-funded PhD student Anna-Claire Devlin, based at the University of St Andrews, has identified that loss of nerve signalling may be an early sign of MND.
Under the leadership of Dr Gareth Miles and Prof Siddharthan Chandran (University of Edinburgh), Anna-Claire measured the nerve impulses in stem cell derived human motor neurones and identified that the ability to send a nerve impulse is impaired during the early stages of the disease.
How a motor neurone works
In order to understand what goes wrong in MND, we need to understand how a motor neurone works.
Motor neurones send signals via electrical impulses from the brain to the muscle, which results in movement. This electrical impulse is known as an ‘action potential’.
This makes motor neurones a bit like telephone wires, allowing the brain to communicate with a specific muscle. For example, the brain will send a nerve signal via a specific motor neurone to a specific muscle cell (eg in the arm). This is a bit like dialling a phone number, each number is unique, allowing the brain to communicate with a specific muscle cell.
In our telephone analogy, once the signal reaches the muscle, the muscle answers the telephone call and does what the brain asks – moves the required muscle.
But how do you measure the electrical signal produced from one motor neurone? Well, Anna-Claire uses a technique that is very similar to pinching the skin on the back of your hand – only they pinch the membrane of a motor neurone!
Anna-Claire explains more: “For our studies, we use a technique called whole-cell patch-clamp recording, which allows us to record the electrical activity of motor neurons and detect possible changes in the specialized membrane proteins, which are necessary for producing action potentials.
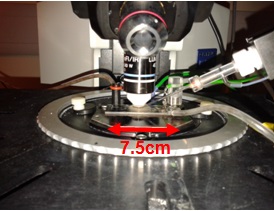
“The experimental set-up includes: a recording chamber – this is where the cells are placed and supplied with oxygenated artificial cerebral spinal fluid, mimicking their normal environment. A microscope lens, which is submerged in the artificial cerebral spinal fluid, is used to visualize motor neurons on the microscope slide (7.5cm) we wish to record from. Small glass capillary tubes (pipettes) with very fine tips are then attached to motor neurons under the guidance of a very finely controlled micro-manipulator.
“The pipette on the manipulator is moved towards the recording chamber, beneath the microscope lens and down towards the motor neuron. Once the neuron and the pipette tip are in focus together, the pipette tip is moved towards the surface (membrane) of the cell and is gently pushed up against it.
“Suction is applied to the pipette, which pulls the membrane of the cell up into the pipette. Once a tight seal is formed between the cell membrane and the pipette, the membrane is broken by further suction so the inside of the cell is continuous with the inside of the pipette. This enables us to record the electrical signals (action potentials) in the motor neuron, which are required for muscle contraction.
“These electrical signals obtained from the motor neurons are then amplified and recorded on a computer.”

What this research means to people living with MND
Anna-Claire said: “We used stem cells derived from skin samples, which we obtained from people living with MND and healthy individuals. Our research found that, even before the motor neurons showed any signs of physical damage, those affected by MND lose the ability to generate the electrical signals that are required to make muscles contract.
“This early loss of function is associated with changes in specialised proteins called ion channels that generate electrical signals in motor neurons. These findings suggest that loss of appropriate electrical signals may be an early step in the disease process and highlights ion channels as potential targets for future therapies.
“Our work also demonstrates that studies of the function of stem cell-derived motor neurons are likely to be important for the development and testing of future drugs aiming to treat and eventually cure MND.”
More about this research:
Dr Gareth Miles (University of St Andrews) and Prof Siddharthan Chandran (University of Edinburgh) were awarded £40,769 in funding by the Association in 2013.
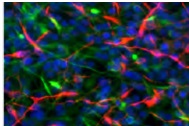
Over the course of two years, Anna-Claire will use cutting-edge technology to turn skin cells donated by people with MND and unaffected people into motor neurones and other types of cells found in the spinal cord in a laboratory dish.
Anna-Claire will also record the electrical activity of the resulting motor neurones, interneurones and support cells. This approach will allow this research group to directly assess the function, and dysfunction, of human, MND-affected motor neurones and their connections with other nearby cell types.
With increasing evidence of changes in the communication between motor neurones and their neighbouring spinal cord cells in MND, this research group expects their direct analyses of human spinal cord cells to reveal important new targets for the development of novel treatments.
Reference:




I have a few questions in regard to how to measure an action potential in a live patient. Can you give me a name of someone who can help.
Thank you
Dr. Crabtree
Dear Dr Crabtree,
You may wish to email the researchers mentioned in this article directly – they might be able to provide further guidance.
Best Wishes,
Martina