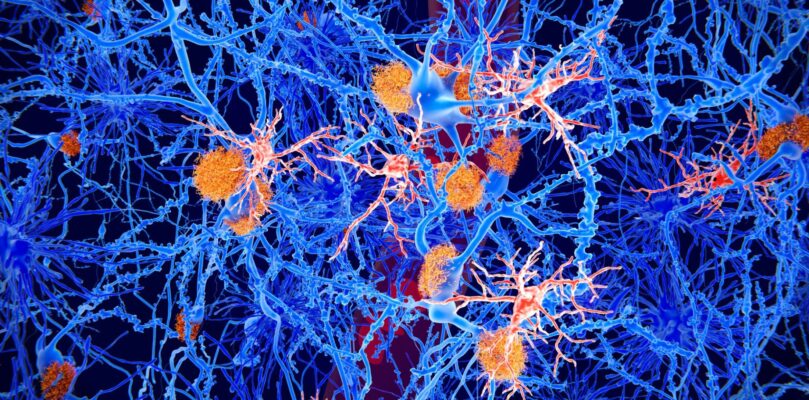
Recent research, led by scientists at the University of Edinburgh and University of Dundee, has identified abnormalities in a type of brain cell called microglia in MND associated with mutations in the C9orf72 gene. It has been suggested for a long time that motor neurons may not be the only type of cell involved in MND, and that damage to other cells in the brain may also be happening in the disease. As well as this, previous research has revealed that the immune system might be over-active and behave abnormally in MND. This study looks into both of these areas using cutting edge stem cell technology to create microglia (brain immune cells) from people with MND who had a mistake in the C9orf72 gene. This work has helped to shed more light on how the C9orf72 gene change may affect the behaviour of microglia, which could be involved in the death of motor neurons in MND.
What are microglia?
Glia are cells that surround motor neurons and provide them with support and nourishment. One type of glia are microglia, which are the main immune cells that patrol the brain and spinal cord. They are constantly looking out for signs of damage and infection to help to protect the neurons from these and maintain a healthy environment in the central nervous system.
What did this work focus on?
The researchers wanted to investigate whether mutations in the C9orf72 gene had an effect on the functions of microglia and if changes in their function or behaviour might contribute to the damage and death of motor neurons seen in MND.
To do this, they used biological samples from people with MND, who had the C9orf72 gene mutation, to create microglia-like cells in the lab. These cells were then compared to healthy microglia cells to look for differences.
As well as looking for changes in microglia in MND, they also wanted to see if any of these changes had an impact on the health of surrounding motor neurons. The researchers created co-cultures, where more than one cell type is grown in a dish in the lab, of microglia and motor neurons which they used to observe interactions between the two cell types. This helped them to see whether the interactions between these cells are altered in C9orf72 MND.
Why was this research needed?
It has previously been suggested that microglia play a role in the development and progression of MND, but it is still unclear how they might be involved in the disease process. By uncovering changes that happen in Microglia in MND, we can increase our understanding of the role they may play in underlying mechanisms of the disease and potentially identify new targets for the development of possible treatments.
What is the cellular wast disposal system?
Our cells have a process in place for recycling old and damaged parts of cells and this process is called autophagy. During this process, worn out parts of the cell are broken down and anything that can be reused is incorporated into new components in the cell. The bits that can’t be recycled are removed from inside the cells and transported to the surrounding environment, where it is taken up by microglia who break it down and dispose of it.
What did the study find?
The researchers studied the C9orf72 microglia-like cells and discovered that less of the C9orf72 protein was being made in these cells. To find out more about the effect that this has on the function of the microglia, they looked at the other proteins that C9orf72 usually interacts with and a number of these proteins were found to be involved in the autophagy process. This suggests that the C9orf72 protein plays a role in controlling the waste clearance process in microglia.
It was observed that less cellular waste was being taken up by microglia with the C9orf72 mutation and levels of two compounds (p62 and LC3) involved in kickstarting the autophagy process were reduced. This shows that there is less autophagy happening in microglia in C9orf72 MND and that there may be errors occurring in the initiation of this process. The researchers were also able to demonstrate that the impaired autophagy seen in C9orf72 microglia also plays a role in the death of motor neurons.
The autophagy process usually helps to reduce responses of the immune system and inflammation because the waste is removed and not left to build up inside the cells. The researchers looked into how reduced autophagy in microglia in C9orf72 MND might affect the action of the immune system. They activated the immune system in healthy and MND microglia to observe differences in responses. In the healthy microglia, the immune system response increased and then decreased as autophagy was activated. However, in the C9orf72 microglia, the response increased and remained high. This supports the earlier findings that autophagy is not activated as it should be and suggests that the immune system response and inflammation are over-active in MND.
Following these findings, the researchers wanted to see whether boosting the activation of autophagy could help reduce these effects. They treated the microglia with an existing drug, called Rapamycin, which is known to activate autophagy and is currently used to treat some cancers and help prevent transplant rejection. Treatment with the drug lead to an increase in the autophagy process and helped to reduce the immune response and inflammation in the C9orf72 microglia. They also found that treatment with Rapamycin led to an increase in motor neuron survival in co-cultures of motor neurons and C9orf72 microglia.
The researchers studied other immune cells from the blood to uncover whether these findings were specific to microglia. They took blood samples from people with the C9orf72 mutation to collect another type of immune cell called macrophages, which have the same role as microglia but are found throughout the body. Researchers found that these cells also displayed a reduction in autophagy and increased inflammation, suggesting that other immune cells are also affected in MND. When these macrophages were treated with Rapamycin, inflammation was reduced, and initiation of autophagy increased. This suggests that these defects are not specific to the brain and are also seen in immune cells throughout the body.
What does this mean?
This research has helped to shed more light on the role that microglia and other immune cells might play in the development and progression of MND. The researchers have discovered one of the underlying mechanisms of abnormal microglia function in the disease, and identified a potential target for future therapy development. By demonstrating that these harmful effects can be reduced using drugs that boost autophagy, they have found a potential strategy to rescue some of these defects. This needs to be tested further in the lab to see whether Rapamycin, or other similar drugs, may be beneficial for MND and could be taken forward for future clinical trials.
What are the next steps for this research?
The researchers are planning further work in this area to highlight more about the role of microglia in MND. These more detailed studies could uncover more abnormalities in the function of microglia in the disease and help to identify more potential drugs that could be beneficial in MND and may be progressed to testing in clinical trials in the future.
This study provides some hope for the development of new therapies for people with MND targeted at glial cells. However, it is important to recognise that a breakthrough in the laboratory takes time to translate to the clinic. This is now our priority.
Professor Siddharthan Chandran, lead author of the study and Director of the Centre for Clinical Brain Sciences, Edinburgh Neuroscience, the Euan MacDonald Centre and the Anne Rowling Regenerative Neurology Clinic.
Arpan Mehta, one of the authors on this paper, is a former Lady Edith Wolfson clinical fellow and was funded by the MND Association.
Resources: