The current pace of clinical trials means that there are now more trials testing potential drugs for MND in the UK than ever before. One of these trials is MND-SMART which is designed to run for several years and give more people with the disease a chance to take part in a trial. The MND Association are proud to be supporting the continuation of this trial through a partnership with MND Scotland.
What is MND-SMART?
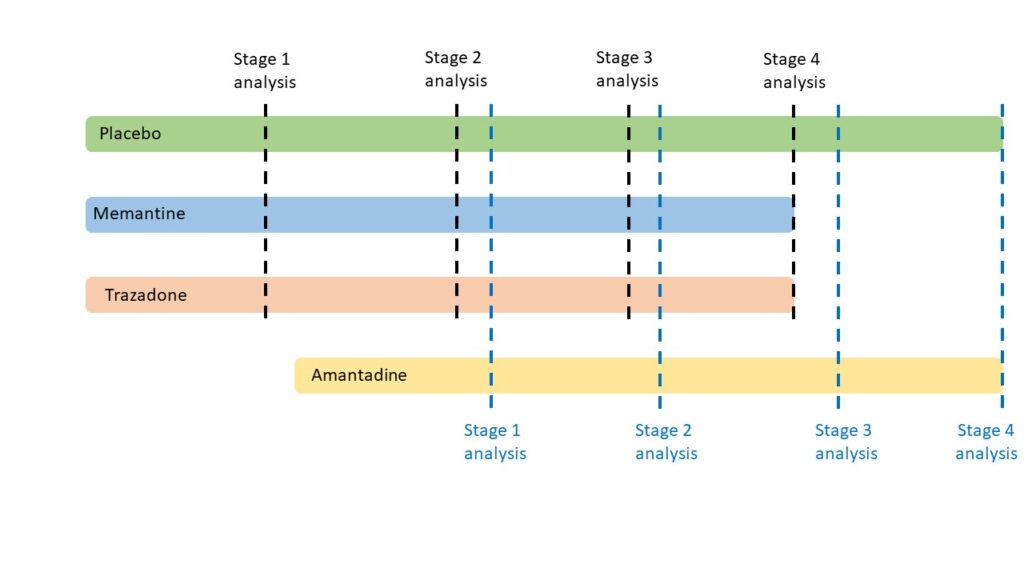
MND-SMART, the UK’s first platform trial in MND, is a long-term study led by the Euan MacDonald Centre at the University of Edinburgh that will run continuously over many years. It is designed to test more than one treatment at a time and is adaptive. This means that researchers can change the drugs being tested throughout the trial, allowing new ones to be added and drugs that are found to have no benefit to be quickly removed. MND-SMART has been running for three years now and over 500 people have already been recruited to take part in the trial. Trial participants taking one of the treatments will be compared with a single group who receive a placebo (a dummy drug). This means that people in MND-SMART are more likely to be randomised to receive an active treatment when compared to other clinical trials, where typically half of the participants receive the placebo and half the active treatment.
What drugs are currently being tested?
There are currently three drugs being tested, including a recently added drug. These drugs are all repurposed drugs as they are already known to be safe and effective for use in other conditions, but they are now being tested to see if they could be beneficial for people with MND. The three drugs currently being trialled are:
- Memantine
- Trazodone
- Amantadine
Memantine is already used to treat Alzheimer’s disease. It works by reducing the action of glutamate which is a neurotransmitter that helps nerve cells to communicate. In MND it is thought that glutamate can be over-active and may be toxic to neurons, contributing to their death.
Trazodone is currently licensed to treat anxiety and depression. It is thought to help protect neurons as it works by slowing the production of faulty proteins. The accumulation of these faulty proteins is toxic to neurons and may play a role in cell death in MND.
Amantadine is a drug which is already used in the management of Parkinson’s disease, treatment of fatigue in Multiple Sclerosis and as an antiviral medicine in the treatment of Type A influenza. It works in a number of different ways including interacting with neurotransmitter signalling pathways in the brain. It is known to help boost the action of one neurotransmitter called dopamine and reduce glutamate activity. In MND, it is thought that over activity of glutamate can be toxic and cause cells to die. Dopamine is an important neurotransmitter involved in motor control and boosting this might help to improve signalling between motor neurons. Previous laboratory studies conducted at the UK Dementia Research Institute in Edinburgh have suggested that amantadine might be effective in reducing the abnormal ‘clumping’ of the TDP43 protein in cells. These protein clumps are known to accumulate within the neurons in around 97% of people with MND and are thought to play a role in the onset and progression of the disease.
RELATED POST
Blog | 02 February 2023 | Eleanor Green
MND clinical trial updates to keep an eye out for in 2023- part 1
How are these drugs tested for positive signs throughout the trial?
MND-SMART is designed with regular monitoring in place for each drug to assess whether to continue testing that drug. This means that drugs which aren’t showing positive signs can be removed at specified time points during the trial. This kind of adaptive trial design means that people with MND aren’t continuing to take a drug which is showing no benefit. These participants can then go on to take part in another trial or be randomised to another drug within the same trial.
For each drug tested in the trial there are 4 time points where the data collected is analysed. This is done to see if positive trends can be seen in order to make the decision to continue testing the drug. You can find out more about these below.
Stage 1 analysis
Stage 2 analysis
Stage 3 analysis
Stage 4 analysis
How are new drugs chosen?
New drugs are selected for the trial based on a continuous review of constantly updated scientific evidence. This includes automated searching of hundreds of scientific publications written by doctors and scientists worldwide. This review also considers results from laboratory studies that test drugs using state-of-the-art human stem cell-based drug discovery platforms. The evidence is regularly reviewed by a drug selection committee, which includes clinical experts on MND, who then decide whether to add a new drug to the trial.
How will these three drugs be tested?
Participants are being recruited to all three drugs and the placebo. Each drug will recruit over 170 people. The placebo will continue to run alongside these, and some people will be randomised to this. While people are being recruited to all three drugs and placebo, participants will be randomised in a ratio of 3:1 for treatments to placebo. Once the testing of memantine and trazadone ends, the testing of amantadine and the placebo will continue.
How can you get involved?
MND-SMART is currently recruiting at several sites throughout the UK and a full list of these centres can be found here. You can register your interest in taking part in the trial using the button below.
If you register your interest the research team will be in touch when there is a place available at a site in your area. Please bear in mind that there might be a wait for the team to contact you.
Platform trials, like MND-SMART, that provide lasting infrastructure for trials and test several possible treatments at once may play a key role in finding new effective therapies. The MND Association are happy to be supporting such an innovative clinical trial and our funding will help maintain the infrastructure to enable MND-SMART to test new drugs for years to come.
Clinical trials like MND-SMART wouldn’t be possible without the dedication, generosity and commitment of researchers, health care professionals and the MND community. Thank you to everyone who is involved in the set-up and running of the trial, and to those with MND who are participating.
MND-SMART is funded by the Euan MacDonald Centre for MND Research, MND Scotland, My Name’5 Doddie Foundation and the MND Association.
* The information in this blog was correct at the time of publication.