Hi, my name is Avril Mc Tague. I am undertaking a Ph.D. at Trinity College, Dublin, Ireland as part of the Multidisciplinary Innovation and Research Advancing Neurological care in a Digital Age (MIRANDA) doctoral award programme. This is funded by the Health Research Board in Ireland. I was one of five symposium communication ambassadors at last year’s international symposium. This blog contains highlights from the technology and telemedicine session. This session included five excellent presentations from experts on how technology and telemedicine can play a role in MND care and research.
What is Telemedicine?
Telemedicine is the use of technology to provide and enhance healthcare. This technology ranges from the use of mobile applications, wearable devices/sensors, like watches, to completing assessment tools, for example, breathing tests, away from the hospital or clinic setting. This is an exciting area in MND as telemedicine can provide the opportunity for people to receive healthcare and take part in research from the comfort of their own home. This may lead to improving the quality of care received by people living with MND, their families, and caregivers.

RELATED POST
Blog | 22 February 2022 | Charlotte Roy
How technology can play a role in connecting the people you love
Contactless Digital Biomarker for Monitoring MND Disease Progression
The first presenter, Dr Crook-Rumsey a post-doctoral researcher at King’s College London and Imperial College London, presented on the use of contactless digital biomarkers for monitoring the progression of MND. A biomarker is a measure that captures what is happening in the body. A digital biomarker captures information on heart rate, breathing rate, and activity levels through a digital device like a wearable sensor, for example, an activity watch, or a sensor, for example, a sleep mat. Often capturing this information requires frequent and lengthy clinic visits. This can create a challenge in monitoring how MND progresses over time. Using remote monitoring devices can capture this information away from the hospital making it more convenient for people living with MND.
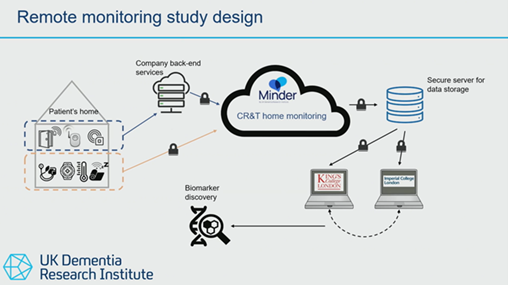
Dr Crook-Rumsey focused on the findings from a research study using a sleep sensor mat to monitor people living with MND. The sleep sensor is placed under the mattress. This sensor measures time in and out of bed, breathing rate, heart rate, and sleep stages. This information is transmitted to the Minder home monitoring platform. The picture below shows how the devices in the person’s home connect to the Minder platform which then transmits the information securely to the research centres. This allows the person to participate in research from the comfort of their own home. The platform was originally developed for people living with dementia.
Dr Crook-Rumsey presented the findings from sixteen people living with MND who used this sleep sensor for 6 months. The findings showed that people living with MND spent less time in bed, and their breathing rate increased while in bed over time compared to data from 12,460 people who did not have MND. These findings highlight how several measures can be taken remotely in MND and how the use of a sleep sensor may, in the future, play a role in monitoring the impact of current or new treatments in MND. This could allow clinicians to respond more quickly to the changes they are seeing in these remote monitoring systems.
If we are taking more convenient regular measurements, we can increase our confidence in the measurement that we are actually taking.
Dr Crook Rumsey
Home-based Assessment in MND
Dr Mueller, an associate director, and principal data scientist with Novartis, presented the initial findings from a study on home-based assessments in MND. Thirty-three people living with MND completed weekly home-based assessments as well as in-clinic assessments every 2-3 months. Participants completed the weekly assessments using a tablet, see the picture below from Dr. Mueller’s presentation. These assessments looked at a number of different functions, like speech, breathing, and hand movement.
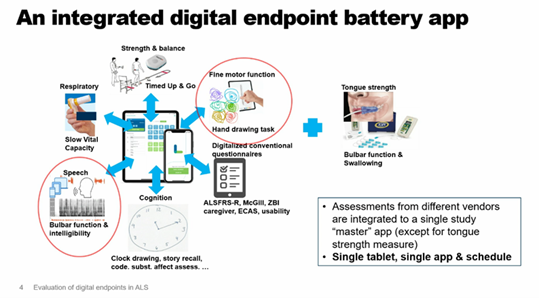
The researchers found that the number of weekly assessments completed by the participants reduced throughout the study. The researchers also found that there was a strong association between the ALSFRS-R score completed remotely in the person’s home and in the clinic. Researchers and clinicians use the ALSFRS-R scale to measure physical function in MND. The strong association found between the remote and clinic ALSFRS-R score, highlights that there may be an opportunity for people living with MND to complete this score in the comfort of their own homes. Interestingly, the participants found the digital technologies easy to use. More research is now needed to identify how frequently tests should be completed as well as ensuring that these tests are useful and meaningful for people living with MND.
Site and Participant Perspectives on the COURAGE-ALS trial design
Dr Runicki, a Professor of Neurology as well as vice president of research and development at Cytokinetics, presented the findings from a study reporting on the views and experiences of the participants and the research sites taking part in the COURAGE-ALS trial. This trial took a new approach to research trial design in MND. The researchers designed the trial so participants could complete the trial in the traditional face-to-face format or remotely using digital technologies. The participants could change from face-to-face visits to remote visits if needed throughout the study. This trial design aimed to make it easier for people living with MND to participate in the trial. The COURAGE-ALS trial investigated the use of a drug called Reldesemtiv in MND. Unfortunately, this study was stopped in March 2023 as this drug showed no evidence of effect on MND.
The researchers in the participating sites completed a survey on their experience of this trial design. Of the 141 responses, 86% of the researchers reported that participants changed from an in-clinic visit to a remote visit. The main reasons given were disease progression, difficulties with transport, caregiver availability, and the weather. The researchers identified a number of challenges to completing breathing assessments remotely. These included the use of technology, hand weakness, and facial weakness.
Fifty participants also completed interviews on their experience of participating in this trial design. Some participants reported having difficulty measuring their breathing function due to internet connectivity issues or not getting an accurate reading. Both the site researchers and participants positively favoured the remote aspect of the COURAGE-ALS trial. The data collected from the COURAGE-ALS trial, especially in terms of trial design, will be useful for researchers who are thinking of planning an MND clinical trial with a remote aspect. It is hoped that this data may help create clinical trials that are even more attractive and easier for people living with MND to be involved in.
Moving Forward
This is an exciting time in technology and telemedicine in MND care and research. Participants across the studies presented at the session reported finding technologies such as sleep and respiratory sensors, easy to use, and convenient while reducing the travel time to hospital appointments. This highlights the potential of this technology in assisting researchers and clinicians in monitoring MND. However, as mentioned by Dr Hobson, a Consultant Neurologist at the Sheffield MND Care and Research Centre and a senior lecturer at the Sheffield Institute at the University of Sheffield, we need to be aware of the challenges when using technology for improved care outcomes. These include the complexity of the condition, limited resources, as well as ensuring that digital technology is acceptable to the people using it. It will be exciting to see how the area of technology and telemedicine in MND continues to develop, potentially leading to an improvement in the quality of care received by people living with MND, their families, and caregivers.
For more information on these presentations, see pages 12-14 in the platform presentations abstract for the conference.
We would like to thank Avril for being a Symposium Communications Ambassador. You can follow Avril on Twitter/X here.